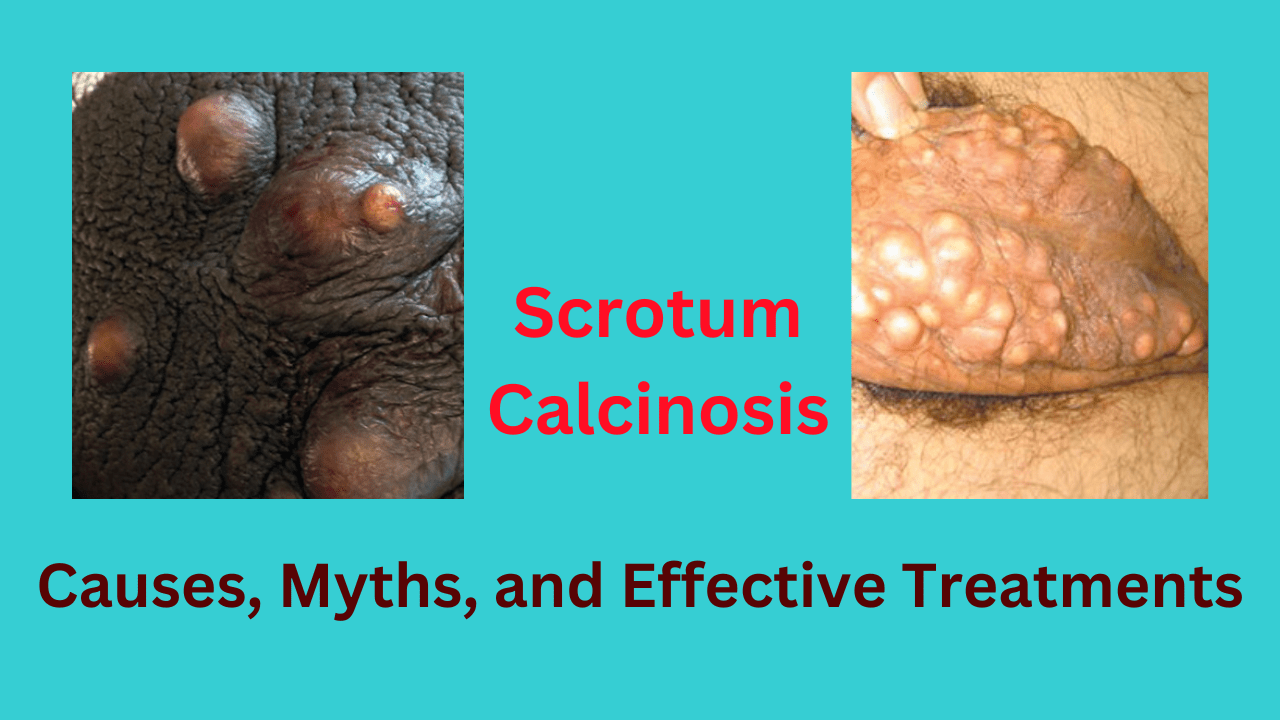
Scrotal calcinosis is a rare benign condition characterized by the presence of calcium deposits in the scrotal skin. The exact cause of scrotal calcinosis remains uncertain, but there are several theories and factors believed to contribute to its development. Here’s a summary of key perspectives on its causes and advances in treatment:
1. Theories Behind Scrotal Calcinosis
- Sebaceous Cyst Theory: One of the widely accepted theories suggests that scrotal calcinosis originates from the degeneration of sebaceous cysts in the scrotum. Over time, these cysts may undergo dystrophic calcification, where calcified material accumulates in the area due to cell breakdown, eventually leading to the formation of scrotal calcinosis.
- Calcium Metabolism Theory: Another hypothesis proposes that disturbances in calcium metabolism may contribute to calcinosis. However, studies have not consistently shown abnormalities in systemic calcium or phosphate levels among individuals with scrotal calcinosis, making this theory less conclusive.
- Genetic Predisposition: While scrotal calcinosis is generally not hereditary, there may be a genetic predisposition to sebaceous cyst formation in some individuals, indirectly contributing to the condition. Research on a direct genetic link remains limited and inconclusive.
- Hair Growth and Minor Trauma: It has been suggested that hair follicles in the scrotal area and minor, repeated trauma might trigger localized inflammation, contributing to calcified deposits over time.
2. Relation to Sebaceous Cysts and Hair Follicles
Scrotal calcinosis is closely related to sebaceous cysts, as they are thought to be the origin of calcified deposits in most cases. When these cysts rupture or degrade, calcium builds up in the tissue, leading to visible nodules. In the presence of hair follicles or minor skin trauma, these cysts may be more likely to form, thus potentially increasing the risk of calcinosis in areas with denser hair or more frequent irritation.
3. Permanent Solutions and Surgical Treatment
- Surgical Excision: Currently, the primary and most effective treatment for scrotal calcinosis is surgical excision. The calcified nodules are carefully removed while preserving the surrounding scrotal skin and tissue. This approach generally provides a permanent solution, as the nodules do not usually recur if completely excised.
- Minimally Invasive Techniques: Newer surgical techniques include smaller incisions and improved suturing methods to minimize scarring and enhance cosmetic outcomes. However, these methods are still in the realm of traditional surgical approaches rather than novel therapies.
4. Recent Advances in Treatment and Research
- Laser Therapy: While not common, some reports suggest laser therapy may be useful for superficial cases. However, the depth of calcifications in scrotal calcinosis often requires more invasive surgical approaches.
- Genetic and Molecular Research: Advances in dermatology and molecular pathology are gradually enhancing the understanding of calcification processes, though direct genetic interventions for scrotal calcinosis have not yet been developed.
- Topical Treatments: Research is ongoing regarding potential topical treatments that could help prevent calcification in sebaceous cysts before they become problematic. However, none are approved specifically for scrotal calcinosis at this time.
While surgical excision remains the definitive treatment, research into understanding the metabolic and cellular processes involved in calcinosis could one day open up non-surgical treatment options. For now, those affected are advised to monitor any nodules and consult a specialist if symptoms arise.
1. What causes scrotal calcinosis?
Scrotal calcinosis is primarily believed to result from the calcification of sebaceous cysts in the scrotal area. Over time, these cysts may break down, leading to the deposition of calcium in the tissue. Other possible causes include minor trauma, inflammation, or repeated friction, which can trigger localized calcification. However, systemic calcium and phosphate levels in individuals with this condition are generally normal, suggesting a more localized process rather than a systemic disorder.
2. Is there a genetic link to scrotal calcinosis?
There is no direct evidence of a genetic inheritance pattern for scrotal calcinosis. However, genetic predispositions to sebaceous cyst formation may play an indirect role. Current research hasn’t identified specific genetic mutations linked to this condition, but individuals with a family history of sebaceous cysts or other benign skin growths may have a slightly increased risk.
3. How is scrotal calcinosis treated?
The most effective and permanent treatment for scrotal calcinosis is surgical excision, where the calcified nodules are removed. Surgeons aim to preserve as much healthy skin as possible to maintain the area’s function and appearance. After excision, the nodules generally do not recur, making surgery a reliable option for most patients. Non-surgical options, like topical treatments, have not proven effective.
4. Are there any recent advances in treating scrotal calcinosis?
Advances in minimally invasive surgical techniques have improved outcomes for scrotal calcinosis patients, minimizing scarring and improving cosmetic results. Some reports mention the potential of laser treatments, although these are more experimental and not commonly used due to the depth of calcifications. Research into the cellular processes that lead to calcification is ongoing, and this may eventually lead to non-surgical treatments in the future.
5. Is scrotal calcinosis related to calcium metabolism disorders?
Generally, scrotal calcinosis does not stem from calcium metabolism disorders. Most patients with scrotal calcinosis have normal serum calcium and phosphate levels. The calcifications are considered “dystrophic,” meaning they occur in damaged or degenerating tissue rather than due to systemic calcium imbalances. Thus, it is more of a localized phenomenon rather than a metabolic disorder.